Hospitals and physicians have used a service line approach for decades to provide efficient, high-quality care to well-defined, patient populations:
Adapted from the product line approach used by other industries, service lines organize all the care that particular patient populations need. For example, an orthopedic service line would provide the various services that joint replacement patients need, beginning 30 days before surgery to 90 days after (i.e., preadmission testing, surgery, and rehabilitation). But leaders often struggle with a common question: “How can we help a service line grow and prosper?”
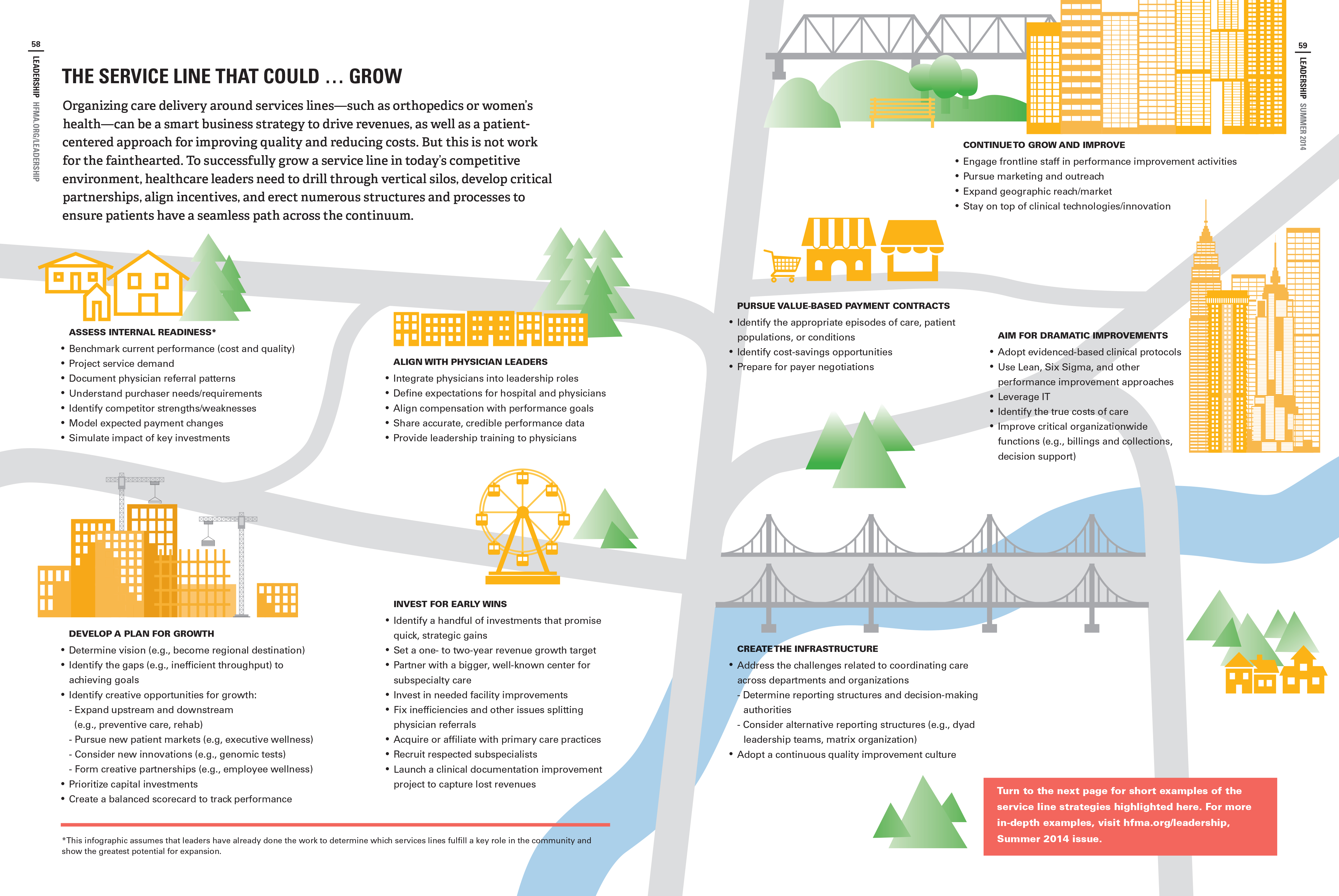
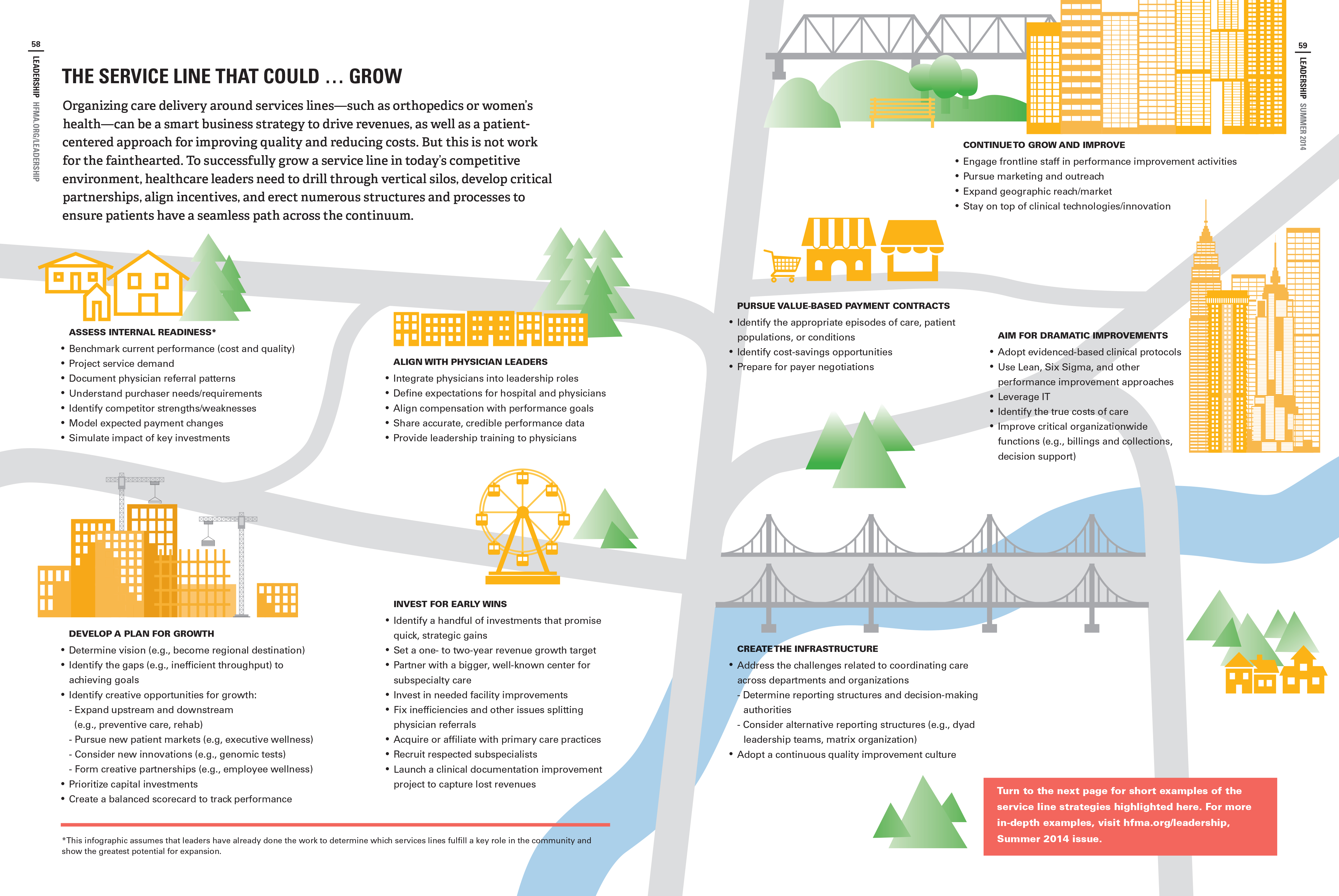
Click on the infographic below, which highlights key steps and examples to consider on this journey.
In recent years, amidst consolidation, major reimbursement cuts, and other disruptive changes, healthcare organizations have been reevaluating their service line offerings. Recognizing that it may not be realistic to be all things to all people, many smaller organizations are deciding to become more focused in their offerings. On the other side of the spectrum, large systems are investing major funds into service lines with growth potential as a way of ensuring they can also provide mission-based services needed in the community.
As they pursue service line growth, hospitals and health systems often progress through some or all of the following eight stages—but not necessarily in sequential order. The examples provided below are only intended to show one possible approach to each stage.
Assess internal readiness. Leaders at Memorial Hermann Health System reviewed service line indicators for each of its major service lines to define the most critical barriers to achieving the goals of improved quality, growth, operational excellence, and satisfaction,” according to an earlier hfm article.
Develop a plan for growth. Chester County Hospital decided to broaden and deepen its cardiac surgery services by affiliating with Cleveland Clinic, which is the No. 1 medical center for cardiac surgery in the country, according to a 2011 Leadership article.
Align with physician leaders. Under a co-management agreement, physician leaders helped save Indiana’s Columbus Regional Health about $250,000 in surgical expenses, while boosting OR start times and employee satisfaction, according to an earlier HFMA CFO Forum article. Physicians are compensated based on a percentage compliance with established metrics and goals.
Invest for early wins. When asked how Montefiore Medical Center has generated even a modest profit given its challenging market, CFO Joel Perlman pointed to a number of strategically-driven, community-oriented investments in an earlier HFMA CFO Forum article:
Organize the work. Scripps Health has adopted a horizontal matrix management structure, creating four Scripps-wide divisions that cross over the traditional vertical silos, as detailed in an earlier Leadership article. Clinical service lines report up to the clinical operations division. The matrix management structure led to $48 million in cost cuts and $29 million in revenue increases—in just one year.
Achieve dramatic improvements. A related concept to service line management is the focused factory, which involves developing “a uniform approach to delivering a limited set of high-quality products,” according to Mayo Clinic’s David Cook, the lead author of a May 2014 Health Affairs article. Cook and his colleagues determined that only a minority of cardiac surgery patients at Mayo truly required individualized treatment plans. In contrast, 67 percent of patients experienced better outcomes (i.e., reduced risk of sepsis, pneumonia, and renal failure) when they received focused-factory care, or standardized, evidence-based care.
Pursue value-based payment contracts. As in an earlier Leadership article, Triangle Orthopaedic Associates and Blue Cross and Blue Shield of North Carolina (BCBSNC) are collaborating around bundled payment arrangements for total hip and knee replacements. Using a prospective model, BCBSNC pays a single flat fee to Triangle for each surgery. That fee covers all expenses from 30 days before the surgery to 90 days after. Triangle pays all providers, including the hospital, anesthesiologists, physical therapists, and others. Procedures are performed at North Carolina Specialty Hospital, of which Triangle is a part-owner. Katie: Link to “Partnering Around Value-Based Payment Approaches” that is in the Summer Leadership.
Continue to grow and improve. To engage front-line staff in continuous improvement, Columbus Regional Health uses a gainsharing program to engage front-line surgical employees (e.g. nurses and technicians), as described in an earlier HFMA CFO Forum article. The amount paid out to the employees is based on the percentage of compliance (tiered) with the established clinical performance metrics and protocols.